If you've been struggling with persistent flaking around your eyebrows, scalp, or red patches on your face, you may be dealing with seborrheic dermatitis. This common inflammatory skin condition affects more than half of adults at some point in their lives [1]. But what causes these frustrating symptoms? Evidence points to a microscopic fungus called Malassezia that lives on everyone's skin.
What Is Malassezia and Why Does It Matter?
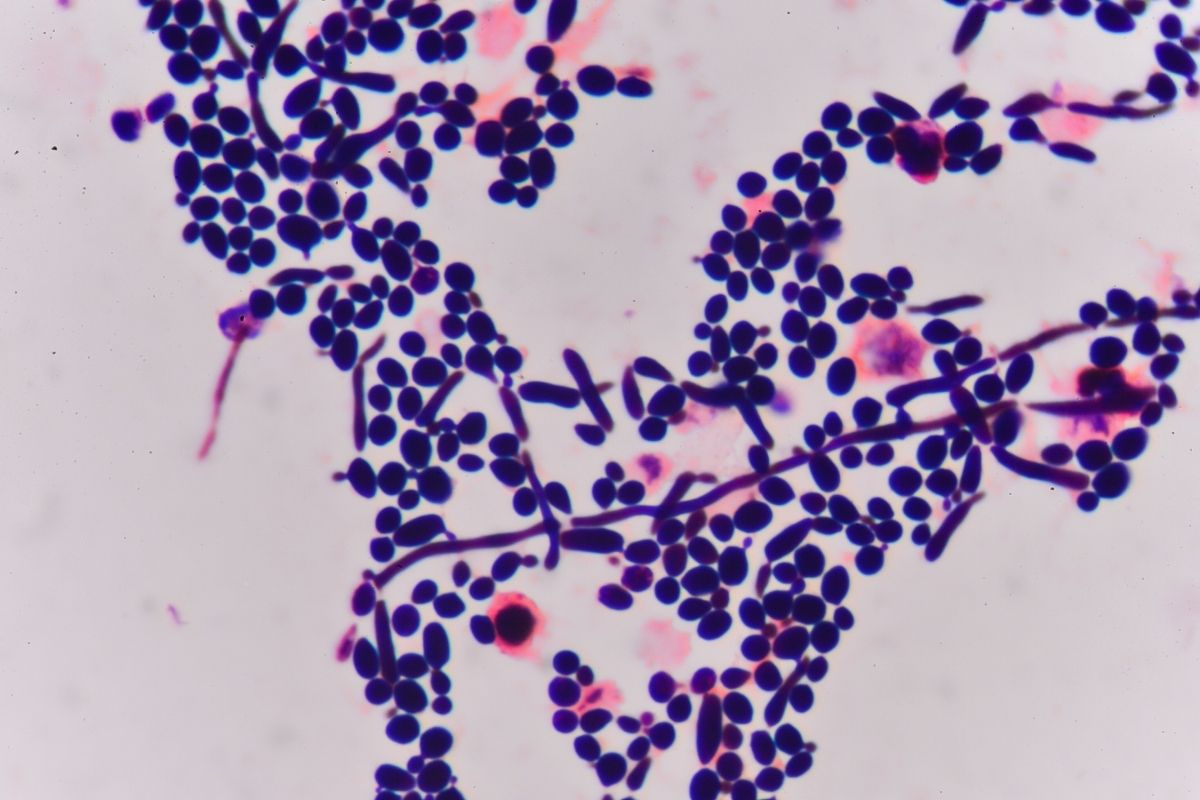
Malassezia is a type of yeast, or fungus, that naturally lives on human skin. It's one of the most abundant fungi found on our bodies, particularly in areas rich in oil-producing sebaceous glands [2]. These include the scalp, face (especially around the eyebrows, nose, and forehead), chest, and upper back.
Here's what makes this fungus unique: Malassezia exists on nearly everyone's skin as part of the normal skin microbiome. In most people, it causes no problems whatsoever. However, in individuals with seborrheic dermatitis, this normally harmless resident triggers an inflammatory response that leads to the characteristic redness, scaling, and flaking [1].
The key question isn't whether you have Malassezia on your skin, as you almost certainly do. The question is why it causes symptoms in some people but not others.
The Three Essential Factors in Seborrheic Dermatitis
Modern research has identified that seborrheic dermatitis develops when three specific factors come together [1]:
-
Sebum production - The oily substance your skin produces
-
Malassezia metabolism - How the fungus processes and breaks down these oils
-
Individual susceptibility - Your unique immune response and skin characteristics
All three factors must be present for seborrheic dermatitis to occur. Understanding each factor helps explain why this condition behaves the way it does.
Why Malassezia Needs Your Skin's Oil
Malassezia has an unusual biological requirement that explains where it lives and how it causes problems. Unlike most organisms, this fungus cannot manufacture its own fatty acids—the essential building blocks all cells need to survive [2]. This limitation comes from the absence of specific genes in Malassezia's genetic code that would normally allow it to produce these fatty acids.
Because Malassezia can't make its own fatty acids, it must obtain them from external sources. This is why the fungus thrives in sebum-rich areas of your body. Sebum, the oily substance produced by sebaceous glands, contains triglycerides and other complex lipids that Malassezia can break down to extract the fatty acids it needs [3].
This dependency on sebum explains the distribution pattern of seborrheic dermatitis. The condition appears where sebaceous glands are most concentrated: the scalp, central face, eyebrows, and upper trunk. Areas with few sebaceous glands rarely develop seborrheic dermatitis because Malassezia populations remain low without their necessary food source.
How Malassezia Breaks Down Sebum
To access the fatty acids locked inside sebum, Malassezia secretes powerful enzymes called lipases and phospholipases [3]. These enzymes act like molecular scissors, cutting apart the complex lipid molecules in sebum into individual fatty acids that the fungus can absorb and use.
This enzymatic breakdown of sebum is where problems begin for people with seborrheic dermatitis. When Malassezia's lipases break down sebum triglycerides, they release both saturated and unsaturated fatty acids. Malassezia preferentially consumes the saturated fatty acids it needs, but the unsaturated fatty acids (particularly oleic acid) are left behind on the skin surface [4].
These leftover unsaturated fatty acids aren't harmless byproducts. Research has shown that oleic acid and other unsaturated fatty acids can penetrate the skin barrier and trigger inflammation in susceptible individuals [4]. Oleic acid has direct irritant effects on skin cells and promotes desquamation (the shedding of skin cells), which creates the visible flaking characteristic of seborrheic dermatitis.
Additionally, arachidonic acid, another byproduct of Malassezia metabolism, serves as a precursor for prostaglandins (inflammatory molecules that cause redness), increased blood flow, and immune cell recruitment [5]. This creates a cascade of inflammatory events that manifests as the red, scaly patches of seborrheic dermatitis.
The Three Main Malassezia Species in Seborrheic Dermatitis
While Malassezia includes at least 18 different species, three specific species are most commonly associated with seborrheic dermatitis: Malassezia globosa, Malassezia restricta, and Malassezia furfur [1][6]. Research consistently identifies these species on the scalp and skin of people with seborrheic dermatitis, though M. globosa and M. restricta tend to be the most predominant, accounting for approximately 90% of isolates from affected skin [8].
What makes these species particularly relevant? Analysis has revealed that M. globosa secretes enzymes specifically designed to break down the complex lipids in sebum [2]. M. furfur has also been documented as an important contributor to seborrheic dermatitis, particularly in certain patient populations and body areas [8]. This genetic adaptation allows these Malassezia species to efficiently exploit the unique ecological niche provided by human skin's oil-rich areas.
Different Malassezia species may produce varying amounts and types of lipases, potentially generating different profiles of irritating fatty acids [6]. This variation might explain why seborrheic dermatitis symptoms can differ from person to person (e.g., some experience primarily flaking, while others deal more with redness and inflammation).
Why the Fungus Affects Some People More Than Others
If Malassezia lives on everyone's skin and breaks down sebum in everyone's sebaceous glands, why do only some people develop seborrheic dermatitis? The answer lies in individual susceptibility; the third essential factor in the condition's development [1].
Research has shown that people with seborrheic dermatitis exhibit altered immune responses to Malassezia and its metabolic byproducts. When the unsaturated fatty acids produced by Malassezia penetrate the skin barrier, they can activate immune cells in susceptible individuals. These immune cells release inflammatory signaling molecules that recruit additional immune cells, amplifying the inflammatory response [7].
In people without seborrheic dermatitis, the immune system tolerates Malassezia's presence and activities without releasing a significant inflammatory response. However, in those with the condition, the immune system perceives Malassezia byproducts as threats, triggering inflammation that leads to the visible symptoms.
The Skin Barrier and Malassezia: A Two-Way Relationship
The skin barrier (the outermost protective layer of your skin) plays an important role in seborrheic dermatitis. A healthy skin barrier consists of skin cells embedded in a matrix of lipids, creating a structure that prevents water loss and keeps irritants out [7].
When seborrheic dermatitis develops, the inflammatory process disrupts this protective barrier. The lipids between skin cells become disordered, and gaps open up in the barrier structure. This disruption has significant consequences for Malassezia-related inflammation.
A compromised skin barrier allows more of Malassezia's byproducts, particularly those irritating unsaturated fatty acids, to penetrate deeper into the skin, potentially triggering more inflammation. This creates a self-perpetuating cycle: Malassezia metabolism causes inflammation, inflammation damages the barrier, and a damaged barrier allows more Malassezia metabolites to penetrate and cause further inflammation [7].
Breaking this cycle requires addressing multiple aspects simultaneously: managing Malassezia activity, supporting the skin barrier, and calming inflammation. This multi-targeted approach is essential for effective management of seborrheic dermatitis.
Managing the Malassezia-Prone Skin Environment
Understanding how Malassezia functions and triggers inflammation in seborrheic dermatitis reveals why effective management requires more than a single approach. The goal isn't necessarily to eliminate Malassezia entirely as it's a normal skin resident that serves ecological functions. Instead, the focus should be on creating skin conditions less favorable for excessive Malassezia activity while supporting barrier function and managing inflammation.
This is where science-driven skincare solutions make a meaningful difference. Octaskin Serum represents this comprehensive approach to managing seborrheic dermatitis. Designed specifically for Malassezia-prone skin environments, the targeted nighttime serum addresses multiple aspects of the condition simultaneously.
By working to reduce surface debris and rebalance the skin's microenvironment, Octaskin Serum targets the factors that allow Malassezia populations to thrive and produce inflammatory byproducts. The formulation supports skin hydration and barrier comfort, which are critical elements for skin dealing with the disruption caused by inflammation. Over time, this approach helps strengthen skin resilience against future flare-ups.
What makes Octaskin Serum particularly valuable is its versatility across all common seborrheic dermatitis areas: the scalp, beard, and eyebrows. Since the condition often affects multiple areas simultaneously, having a consistent, science-based approach simplifies management while targeting the underlying Malassezia-related mechanisms.
How Malassezia Populations Grow in Seborrheic Dermatitis
One consistent finding in seborrheic dermatitis research is that affected skin hosts larger populations of Malassezia compared to normal skin [1]. While Malassezia exists on everyone's skin, the density of fungal cells is significantly higher in areas with active seborrheic dermatitis.
Several factors contribute to this population increase. First, the inflammatory process itself may create conditions that favor Malassezia growth. Inflammation disrupts the normal balance of the skin's microbial ecosystem, potentially reducing competition from bacterial species that would otherwise keep Malassezia populations in check.
Second, when the skin barrier is compromised by inflammation, more sebum and cellular debris may accumulate on the skin surface, providing additional nutrients for Malassezia. This increased food supply supports larger fungal populations.
Third, the rapid turnover of skin cells caused by inflammation creates more dead skin cells on the surface; organic material that Malassezia can colonize. This creates an environment rich in lipids for fungal growth.
The relationship between Malassezia population density and symptom severity isn't perfectly linear as some people with high Malassezia counts have minimal symptoms, while others with moderate counts experience significant inflammation. This variation underscores the importance of individual susceptibility: it's not just how much Malassezia is present, but how your immune system responds to its presence and metabolic activities.
The Sebaceous Gland Connection
Malassezia's dependence on sebum creates a direct connection between seborrheic dermatitis and sebaceous gland activity. Sebaceous glands are microscopic structures embedded in the skin that produce sebum. Their density varies across different body areas, with the highest concentrations on the scalp, face, and upper trunk—exactly where seborrheic dermatitis most commonly occurs [3].
These glands are regulated by hormones, particularly androgens. This hormonal control explains several patterns observed in seborrheic dermatitis:
-
Age distribution: The condition commonly appears in infancy (when maternal hormones are still present), decreases during childhood (when sebum production is low), and increases after puberty (when hormones activate sebaceous glands) [1]
-
Gender patterns: Males often experience more severe seborrheic dermatitis, potentially related to higher androgen levels that stimulate more sebum production
-
Location specificity: Areas with few sebaceous glands rarely develop seborrheic dermatitis
The sebaceous gland connection also explains why seborrheic dermatitis is a chronic, relapsing condition. Sebaceous glands continuously produce sebum throughout life, providing a constant food source for Malassezia. This ongoing sebum production means Malassezia populations can regrow after treatment, and symptoms can return when conditions favor fungal activity and inflammation.
A Comprehensive Approach to Long-Term Management
The science behind Malassezia and seborrheic dermatitis reveals why effective management requires addressing multiple factors simultaneously. Malassezia's metabolism, the inflammatory response it triggers, and the skin barrier disruption that follows all interact to create and perpetuate the condition.
Successful management approaches should:
-
Help manage Malassezia activity without completely disrupting the skin's natural fungal populations
-
Support skin barrier function to minimize the penetration of irritating metabolites
-
Address visible inflammation to break the inflammatory cycle
-
Maintain skin hydration essential for barrier integrity
Octaskin Serum embodies this comprehensive, science-based approach. Formulated specifically for the unique challenges of Malassezia-prone skin, this nighttime treatment works while you sleep—when your skin's natural repair processes are most active.
The serum targets visible flaking and redness while working to rebalance the skin environment that allows Malassezia overgrowth. By supporting hydration and barrier comfort, it addresses the skin disruption that perpetuates inflammation. Over time, this multi-faceted approach helps build skin resilience, making future flare-ups less likely and less severe.
Whether you're dealing with scalp scaling, facial redness, or irritation in your beard or eyebrows, Octaskin Serum provides a targeted solution that works with your skin's biology rather than against it. By understanding and addressing the Malassezia-related mechanisms underlying seborrheic dermatitis, you can move toward calmer, more comfortable skin.
Conclusion: Knowledge Is Power in Managing Seborrheic Dermatitis
Malassezia isn't your enemy—it's a natural part of your skin's ecosystem that, under certain circumstances, can trigger inflammation. Seborrheic dermatitis emerges from the complex interaction between this fungus's metabolic needs, the biochemical byproducts it produces, and your individual immune response.
Understanding the science behind Malassezia and seborrheic dermatitis empowers you to make informed decisions about managing your condition. It's not about finding a single cure but rather about addressing the multiple factors that together create an environment where symptoms develop: fungal metabolism, inflammatory responses, and skin barrier integrity.
The more we learn about how Malassezia functions and interacts with human skin, the better equipped we are to develop effective management strategies. By working with scientifically formulated solutions that target the underlying mechanisms of the condition, you can achieve more consistent, longer-lasting relief from seborrheic dermatitis symptoms.
References
[1] Dawson TL Jr. Malassezia globosa and restricta: breakthrough understanding of the etiology and treatment of dandruff and seborrheic dermatitis through whole-genome analysis. J Investig Dermatol Symp Proc. 2007;12(2):15-19.
[2] Xu J, Saunders CW, et al. Dandruff-associated Malassezia genomes reveal convergent and divergent virulence traits shared with plant and human fungal pathogens. Proc Natl Acad Sci U S A. 2007;104(47):18730-18735.
[3] DeAngelis YM, Gemmer CM, Kaczvinsky JR, et al. Three etiologic facets of dandruff and seborrheic dermatitis: Malassezia fungi, sebaceous lipids, and individual sensitivity. J Investig Dermatol Symp Proc. 2005;10(3):295-297.
[4] Ro BI, Dawson TL. The role of sebaceous gland activity and scalp microfloral metabolism in the etiology of seborrheic dermatitis and dandruff. J Investig Dermatol Symp Proc. 2005;10(3):194-197.
[5] Prohić A, Jovović Sadikovic T, Krupalija-Fazlić M, Kuskunović-Vlahovljak S. Malassezia species in healthy skin and in dermatological conditions. Int J Dermatol. 2016;55(5):494-504.
[6] Hort W, Nilles M, Mayser P. Identification and characterization of lipases from Malassezia restricta, a causative agent of dandruff. FEMS Yeast Res. 2015;15(7):fov078.
[7] Watanabe S, Kano R, Sato H, Nakamura Y, Hasegawa A. The effects of Malassezia yeasts on cytokine production by human keratinocytes. J Invest Dermatol. 2001;116(5):769-773.
[8] Park M, Jung WH, et al. Presence of Malassezia Hyphae Is Correlated with Pathogenesis of Seborrheic Dermatitis. Microbiol Spectr. 2021;9(3):e0116921.